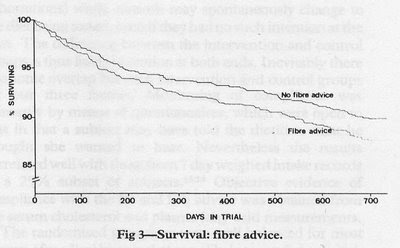
Oops! How embarrassing. At two years, the group that doubled its fiber intake had a 27% greater chance of dying and a 23% greater chance of having a heart attack. The extra fiber was coming from whole grains. I should say, out of fairness, that the result wasn't quite statistically significant (p less than 0.05) at two years. But at the very least, this doesn't support the idea that increasing fiber will extend your life. I believe this the only diet trial that has ever looked at fiber and mortality, without also changing other variables at the same time.
Why might fiber be problematic? I read a paper recently that gave a pretty convincing answer to that question: "Dietary Fibre and Mineral Bioavailability", by Dr. Barbara F. Hartland. By definition, fiber is indigestible. We can divide it into two categories: soluble and insoluble. Insoluble fiber is mostly cellulose and it's relatively inert, besides getting fermented a bit by the gut flora. Soluble fiber is anything that can be dissolved in water but not digested by the human digestive tract. It includes a variety of molecules, some of which are quite effective at keeping you from absorbing minerals. Chief among these is phytic acid, with smaller contributions from tannins (polyphenols) and oxalates. The paper makes a strong case that phytic acid is the main reason fiber prevents mineral absorption, rather than the insoluble fiber fraction. This notion was confirmed here.
As a little side note, polyphenols are those wonderful plant antioxidants that are one of the main justifications for the supposed health benefits of vegetables, tea, chocolate, fruits and antioxidant supplements. The problem is, many of them are actually anti-nutrients. They reduce mineral absorption, reduce growth and feed efficiency in a number of species, and the antioxidant effect seen in human plasma after eating them is due largely to our own bodies secreting uric acid into the blood (a defense mechanism?), rather than the polyphenols themselves. The main antioxidants in plasma are uric acid, vitamin C and vitamin E, with almost no direct contribution from polyphenols. I'm open to the idea that some polyphenols could be beneficial if someone can show me convincing data, but in any case they are not the panacea they're made out to be. Thanks to Peter for cluing me in on this.
Whole grains would be a good source of water-soluble vitamins and minerals, if it weren't for their very high phytic acid content. Even though whole grains are full of minerals, replacing refined grains with whole grains in the diet (and especially adding extra bran) actually reduces the overall absorption of a number of minerals (free text, check out table 4). This has been confirmed repeatedly for iron, zinc, calcium, magnesium and phosphorus. That could well account for the increased mortality in the DART trial.
Refining grains gets rid of the vitamins and minerals but at least refined grains don't prevent you from absorbing the minerals in the rest of your food. Here's a comparison of a few of the nutrients in one cup of cooked brown vs. unenriched white rice (218 vs. 242 calories):
 Brown rice would be quite nutritious if we could absorb all those minerals. There are a few ways to increase mineral absorption from whole grains. One way is to soak them in slightly acidic, warm water, which allows their own phytase enzyme to break down phytic acid. This doesn't seem to do much for brown rice, which doesn't contain much phytase.
Brown rice would be quite nutritious if we could absorb all those minerals. There are a few ways to increase mineral absorption from whole grains. One way is to soak them in slightly acidic, warm water, which allows their own phytase enzyme to break down phytic acid. This doesn't seem to do much for brown rice, which doesn't contain much phytase. A more effective method is to grind grains and soak them before cooking, which helps the phytase function more effectively, especially in gluten grains and buckwheat. The most effective method by far, and the method of choice among healthy traditional cultures around the world, is to soak, grind and ferment whole grains. This breaks down nearly all the phytic acid, making whole grains a good source of both minerals and vitamins.
The paper "Dietary Fibre and Mineral Bioavailability" listed another method of increasing mineral absorption from whole grains that I wasn't aware of. Certain foods can increase the absorption of minerals from whole grains high in phytic acid. These include: foods rich in vitamin C such as fruit or potatoes; meat including fish; and dairy.
Another point the paper made was that the phytic acid content of vegetarian diets is often very high, potentially leading to mineral deficiencies. The typical modern vegetarian diet containing brown rice and unfermented soy products is very high in phytic acid and thus very low in absorbable minerals. The more your diet depends on plant sources for minerals, the more careful you have to be about how you prepare your food.







